Home > Revenue Cycle Management > Medical Coding
Autonomous Coding Backed By Human Expertise
Designed for accuracy, speed, and audit-ready compliance
Preactively Prevent Denials. Accelerate Cash Flow.
AI-driven coding platform that combines autonomous code generation, human validation, and pre-bill compliance reviews to deliver faster claims and fewer denials.
AI-powered autonomous coding for inpatient, outpatient, hospital-based, and professional billing settings
Human-in-the-loop validation catches low-confidence cases before submission, further reducing denials and compliance risks
Integrated pre-bill review safeguards charge integrity and maximizes first-pass payment rates
Compliance monitoring and continuous learning ensure your coding stays smarter and audit-ready with every submission
Coding Excellence That Deliver Measurable Results
Connected Documentation to Coding
Capture complete, compliant documentation with ambient scribe. Better documentation at the source drives coding accuracy and maximizes revenue capture.
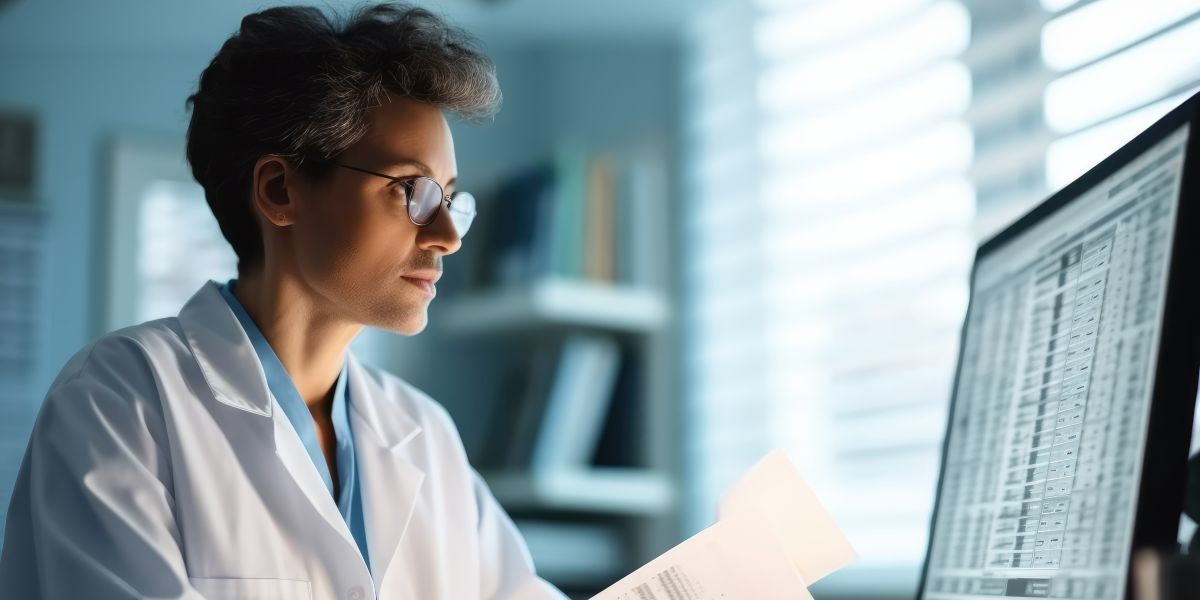
Autonomous Intelligence with Expert Oversight
AI processes charts instantly with confidence scoring. High-confidence cases move to billing; complex cases route to expert coders with AI guidance.

Multi-Layer Compliance Protection
Intelligent pre-bill review validates every claim against revenue rules, medical necessity, and payor requirements before submission.
Scalable, AI-Enabled Workforce
Flexible hybrid model combining AI efficiency with certified coding professionals. Global delivery provides 24/7 coverage and rapid turnaround at scale.
Real Results. Trusted by Leading Hospitals and Health Systems.
We Autonomously Code with Precision. We Audit for Impact. We Optimize for Results.
95%+
Coding accuracy rate
24–48 Hrs.
Turnaround time with full audit trails
SOC2
Compliance and seamless EHR/RCM integration
Built-in Ambient Scribe
Relieves clinicians of administrative burden
Medical Coding Resources
How Managed Medical Coding Services Build Long-Term Stability
Transforming Documentation And Coding While Easing Clinician Burden
Streamlining Revenue Cycle with AI Workflow: Linking Documentation and Coding
Discover Hidden Revenue Opportunities with a Comprehensive Coding Assessment
Our expert team will analyze your coding operations and identify specific areas where you can improve accuracy, reduce denials, and capture missed revenue.