The Evolution of CMS-HCC Models: V28’s Impact on Patient Care and Risk Adjustment

The healthcare industry is continuously evolving, and with it so are the regulations implemented to ensure quality patient care and accurate reimbursement. The Centers for Medicare & Medicaid Services – Hierarchical Condition Category (CMS-HCC) model is no exception, with the latest version (V28) in a three-year phased implementation which started January 1, 2024.
This latest update brings significant changes from V24 as CMS adjusts the model to reflect more current trends, such as recent cost, utilization, and diagnostic patterns. The changes in V28 will impact the risk adjustment factor (RAF) scores, and CMS estimates an overall decrease in payments of 2.45% due to risk model revision and FFS Normalization factor. Understanding the changes, including new HCC categories, coding criteria, and adjustments in risk score calculations, can help enhance your patient health outcomes as well as keep your organization from leaving money on the table.
The Beginning of CMS-HCC
Beginning in 2004, the CMS-HCC model was designed to estimate healthcare costs for a given patient based on their level of risk as a way to provide higher reimbursement to providers caring for higher risk or more complex patients. Each HCC is mapped to an ICD-10-CM code that assigns a RAF score. Patients with lower RAF scores typically have fewer chronic or less serious health conditions and are expected to have average medical costs, while patients with multiple chronic conditions are expected to have higher scores and medical costs.
Properly coded HCCs allow for a more precise picture of a patient’s health status, and can support providers in developing better tailored care plans and proactive management of chronic conditions to improve care quality. Accurate coding also identifies gaps in care and facilitates better monitoring and coordination of treatment, as well as appropriate reimbursement for organizations. AAFP states, “In addition to helping predict health care resource utilization, RAF scores are used to risk adjust quality and cost metrics. By accounting for differences in patient complexity, quality and cost performance can be more appropriately measured.”
With the shift to value-based care, the HCC model is becoming more widely utilized, and CMS continues to adjust the model based on newer available data. CMS reclassified the HCCs to “take into account the clinical classification system changes, disease patterns, treatment methods and their costs, and coding practices, as well as compositional changes within the Medicare population.”
Key Updates in CMS-HCC V28
CMS’ HCC recalibration for V28 has the most significant impact so far. While the overall number of HCCs is increasing from 86 to 115, many HCCs are being remapped and RAF score calculations are changing, including a reduction of RAF scores for commonly coded conditions as nearly 2200 ICD-10 codes no longer map to HCCs. This impact will have a projected 2.16% decrease in average risk scores in calendar year 2024, and a 2.45% decrease in calendar year 2025 for Medicare Advantage (MA) plans. Healthcare organizations will need to adjust their coding practices to align with the new standards to ensure they receive appropriate reimbursements.
The V28 model will be gradually phased in over three years starting in 2024. CMS states that risk scores will be calculated as a blend during this period. In calendar year (CY) 2024, 67% of the risk scores calculated with the current model (the 2020 model) and 33% of the risk scores calculated with the updated model (the 2024 model); while in CY 2025, 33% of the risk scores calculated with the 2020 model and 67% of the risk scores calculated with the 2024 model and in CY 2026,100% of the risk scores to be calculated with the 2024 model.
Some of the key changes from V24 to V28 include:
- 2,200+ ICD-10-CM diagnosis codes removed
- 200+ new ICD-10-CM diagnosis codes added
- Remapping of ICD-10 codes between HCC categories
- Reorganized HCC categories
- Increased HCCs from 86 to 115
- RAF score calculation changes
- Increased specificity in coding and diagnoses
In addition to these changes allowing for more precise coding and reducing misclassification of diagnoses, they will also affect how certain conditions are evaluated. It is now even more crucial for organizations to stay updated in the event any other changes are implemented, be highly specific and intentional in documentation, and adjust coding practices to align with the new standards to avoid improper coding and denials.
Financial Implications from V28 Updates
The Impact on RAF Scores
The changes made to V28 will significantly impact RAF scores, directly affecting reimbursement. CMS states that the modifications will result in “more appropriate relative weights for the HCCs in the model because they reflect more recent utilization, coding and expenditure patterns in FFS Medicare.” V28 focuses on the severity, rather than the number, of medical conditions and uses a constraining process where related HCCs are given the same coefficients. This is intended to capture more complete and accurate data for patients with chronic conditions.
The recalibration of the coefficients may impact the RAF score of a patient without any change in that patient’s health status. For example, a patient with diabetes with chronic complications would have different HCC codes for each variant in V24. In V28, this same patient will receive a lower RAF score without any health changes because now variants related to diabetes all receive the same code and value.
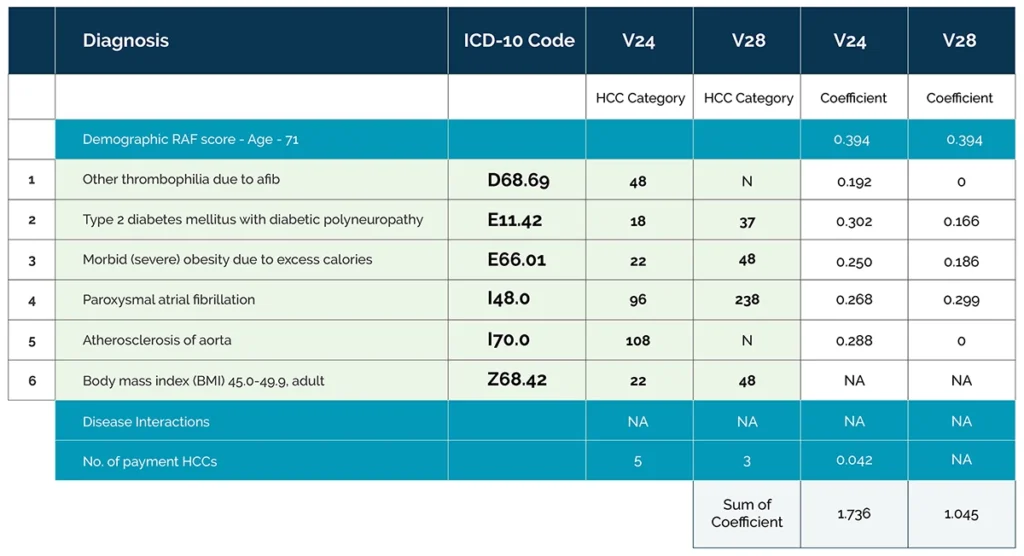
The potential impact of coefficient recalibration on overall RAF score is demonstrated in the example chart below. For a patient with underlying conditions, the RAF score drops from 1.736 to 1.045. Considering a bid rate of $800 PMPM for a location, the risk adjusted payment would have been $1389 in v24 which significantly decreases to $836 in v28 for the same patient.
What V28 Changes Mean for Clinicians and Coding
Not only must clinicians be aware of the various changes to HCC coding and mapping, but the increased specificity requires even more accurate and clinically relevant supporting documentation. With a likely reduction in RAF scores and reimbursement, provider organizations need to plan ahead to be financially prepared. Understanding how V28 will impact reimbursement will help optimize care management strategies, especially for patients with complex and chronic conditions.
Adding to this challenge, clinicians and coders are expected to manage both V24 and V28 risk adjustment models during the three-year phase-in period. This requires a thorough understanding of the different score calculations, what conditions are classified as HCCs each version, and the new codes for those that have been reorganized.
Strategies for a Smooth Transition to V28
Tips for Healthcare Provider Organizations
- Training and Education
Conduct ongoing training sessions with coding and billing staff to familiarize them with the new categories and guidelines. - Review Accepted/Rejected Codes
Needs to look more closely at why front-line clinicians accept or reject codes as rejection of valid codes due to lack of understanding of the guidelines is much more ‘costly - Enhance Documentation Practices
Ensure comprehensive and accurate patient documentation to capture the full scope of patient conditions. - Utilize Advanced Coding Tools
Leverage technology for risk coding solutions to address HCCs, as well as open risk gaps, to ensure they are properly coded. - Stay Informed
With frequent updates to its models and regulations from CMS, it’s important to stay informed of future changes to better prepare as they go live. - Audit and Monitor
Regular audits will help verify coding accuracy and compliance as well as understand how your patients’ updated RAF scores are affecting reimbursement.
Ensure Success in the Transition to V28
The transition from CMS-HCC V24 to V28 brings significant updates with direct implications to RAF scores and reimbursement. Staying informed about the changes, implementing best practices for coding and documentation, and leveraging strategic insights will help ensure a smooth transition. With the right approach, healthcare organizations can navigate these changes effectively, ensuring accurate risk adjustment and enhanced patient outcomes.
Accurate coding, thorough documentation, and continuous education are key to navigating these changes and any future evolutions successfully. As organizations adapt, the focus remains the same: providing high-quality patient care and ensuring accurate compensation for the complexity and scope of care.
Having a partner, like IKS Health, enables organizations to succeed across the risk spectrum by providing precise diagnosis and risk identification, detecting overlooked chronic conditions, and identifying care opportunities, as we did through our Clinical Chart Review program. Our review of over 125,000 records led to a 0.207 improvement in RAF score per patient by identifying more potential condition diagnoses per chart. This resulted in a potential increase in revenue of $74.65M across four healthcare organizations.
IKS also provides a comprehensive platform that pulls together disparate sources to create richer data at point-of-care to connect care, improve health outcomes, and optimize financial performance. With increased support in transitions of care and care coordination and reduced administrative burdens, IKS provides clinicians with the time they need to spend with patients.