Home > Blogs > Key Highlights of the Virtual Scribe and Ambient Speech Competitive Market Insights White Paper
Key Highlights of the Virtual Scribe and Ambient Speech Competitive Market Insights White Paper

The potential for faster, accurate, and compliant clinical documentation that complements rather than disrupts clinical workflow is more important now than ever as the need to remove traditional documentation burdens from clinicians has escalated as the burnout crisis continues. Removing this burden while ensuring quality has led to the evolution of medical scribing over the years with ambient speech solutions being heralded as the new frontier of healthcare technology.
Ambient Gen AI Potential and Cautions
Gen AI provides the documentation of patients in near real time at a fraction of the cost of live or remote scribes. This eliminates any delay from a clinician that might also result in notes that contain recall bias or less detail. Natural language processing (NLP) and automated speech recognition accurately capture the patient-clinician interaction, allowing the clinician to devote more time and attention to their patients rather than the keyboard.
However, Gen AI encounters its own set of challenges, such as the complexities of clinical conversations, background noise, accents, and other language variabilities that can lead to inaccuracies. There are also limitations with understanding emotional nuances, implicit meanings, and other factors that pose risk for omissions, misinterpretations, biases, and hallucinations. This calls for greater oversight — especially because there are gaps in regulation and understanding of the technology — to reduce any risk relating to malpractice, security, and compliance.
Competing Workflow Models
At their core, all competing scribing and ambient speech solutions share the same basic workflow components (Figure 1): capturing the conversation between clinician and patient, converting that input into discrete data in an EHR record, and presenting a ‘draft’ clinical note for review and editing prior to sign off by the clinician. However, how that conversation becomes a document that is ready for review and sign-off, and the completeness and accuracy of what is presented, can vary greatly among these competing workflow models.
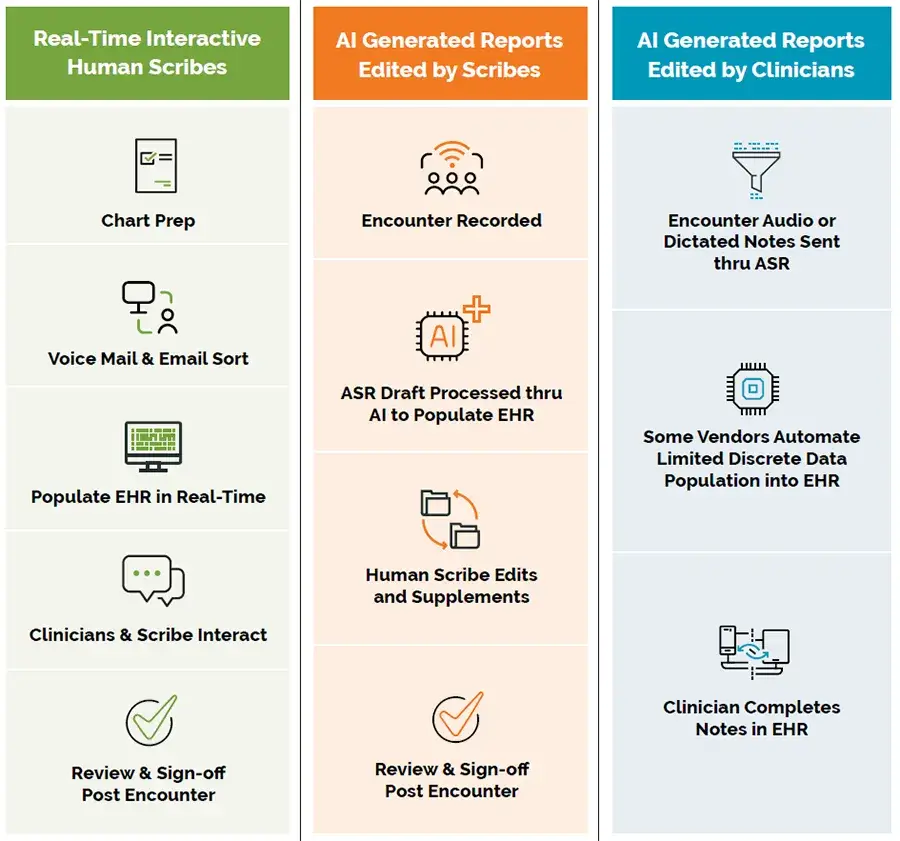
Real-time Scribe Advantages:
- Two-way synchronous interaction with clinicians: Optimizes the quality and application of individual clinician preferences.
- Enables ancillary support: Includes pre-charting, order entry, email/voicemail sorting, and other clerical tasks.
- Best quality for billing and ongoing care: Ensures discrete data capture and eliminates “pajama time.”
- Effectively reduces burnout: By eliminating pajama time.
- Improved documentation quality: Increases RVUs by as much as 12%.
- Documentation efficiency: Allows the ability to see more patients without additional clinic time.
Real-time Scribe Disadvantages:
- Highest price point: Although turnover and pricing concerns can be mitigated by offshoring.
- General inconsistencies: Variations from one scribe to the next can create the impression of scribes being in constant training mode for some clinicians.
- Added documentation expense: For clinicians required to self-document.
- Chronic domestic staff turnover: And back-up availability with some vendors.
- Perceived as a stopgap solution: Pending further development of effective AI.
- Per-note or per-hour charge: May impede ability to accurately budget for costs.
Ambient Speech – Scribe Edited Advantages:
- Properly formatted draft notes: As with live scribes, ambient speech with scribe-supported encounter notes can import and properly place supporting/reference data defined by the clinician. Gen AI content can also be linked to user-selected diagnoses to support downstream charting and coding efforts. Some vendors can also provide order entry, after visit summaries, and other ‘wrap-around’ tasks.
- True documentation creation support with effective burnout relief: Provides substantial relief from documentation burden, reducing clinician burnout.
- Integration with other AI use cases: May pair with other developing use cases, such as automated orders for evidence-based decision support, pattern recognition in clinical encounters to cue unsuspected diagnoses, and sentiment analysis.
- Increases RVUs: Able to increase RVUs by as much as 12% through billing-focused augmented support.
- Predictable cost-modeling: Per-FTE charge allows for more predictable cost modeling.
Ambient Speech – Scribe Edited Disadvantages:
- Complex personal documentation preferences: More difficult to meet complex personal documentation preferences and may not provide ancillary support.
- Variable cost and editing load: Cost and final clinician editing load can be highly variable depending on the AI engine and scribe proficiency.
- No live support of other peri-visit tasks: Does not provide live support for other peri-visit tasks such as pre-charting and managing messages.
- Missed components of clinical assessment: Components of the clinical assessment not captured in conversation may be missed. Depending on the level of scribe support, additional review by the clinician may be required.
- Turnaround time: Longer (but still reasonable) turnaround time compared to real-time solutions.
Ambient Speech – Clinician Edited Advantages:
- Lowest cost entry-level AI clinical documentation capture solution: Easiest to implement with no scribe labor variables involved.
- Strong market growth potential: Due to increased market expectations for AI-based solutions that eliminate human labor.
- Near real-time processing: Efficiently processes EHR notes with decent summarization.
- Integration with other use cases: May pair with other developing AI use cases, such as automated orders for evidence-based decision support, pattern recognition in clinical encounters to cue unsuspected diagnoses, and sentiment analysis.
- Clinician control: Clinicians remain in 100% control of all content details.
- Least impact on reducing the clinical documentation burden: Clinicians must supplement delivered AI content for complete ongoing care and RCM purposes.
- Variable EHR integration capabilities: Accuracy and completeness of conversation capture, as well as formatting/template options, vary between vendors.
- Incomplete documentation: Studies suggest that clinicians who document hours after an encounter tend to not include the same level of documentation details as are typically produced by human scribe-supported workflows.[1]
- Missed components of clinical assessment: Components of the clinical assessment not captured in conversation may be missed.
- Potential loss of malpractice coverage: If a contested issue is traced to AI input, there could be loss of malpractice coverage.
- Risk of payer denials: AI generated notes followed by AI coding maximize risks for payer denials.
- Does not fix chronic compliance issues: AI does not address other poor documentation habits or compliance issues.
What Works Best for Your Practice
One clinical documentation solution may not fit all needs, as different types may be optimal for various pools of clinicians, specialties, and organizations based on personal preferences and comfort with technology, care environment, patient demographic and complexity mix, and the particular content necessary to extract from the clinical visit. Figure 2 offers a framework to match clinician styles and preferences to workflow solutions.
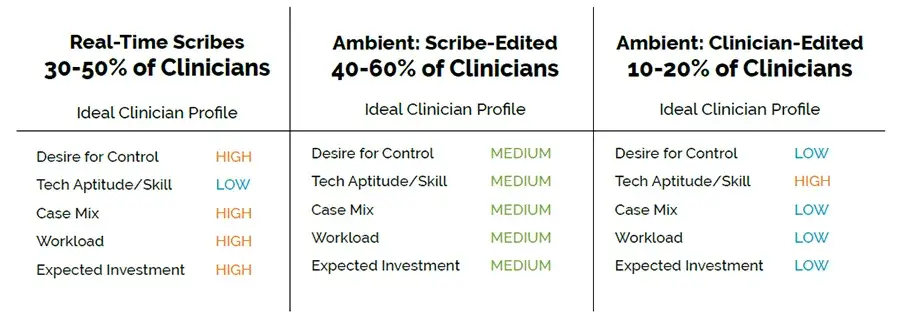
Ambient speech has great potential to be a cost-effective solution to burnout, improve clinical documentation quality, and optimize revenue for a clinic.
The interested party should approach the vendor with a thought in mind of what is best for the practice, relying on “care-driven versus product-driven clinical documentation solutions” as a starting point for these discussions.
While technology undoubtedly introduces significant efficiencies and advantages to many elements and processes of care, it has also been a primary driver of the continued overwhelming burnout experienced by clinicians. Solving tech-driven burnout with even more technology, especially in a complex human-centered industry, cannot be the sole expectation. For clinicians, the majority of whom operate in extremely high stress environments, there are tremendous emotional and operational/workflow advantages to the placement of a human-led processing layer on top of evolving machine learning algorithms, providing ideal care for both patient and clinician.
Discover scribing options that can transform your practice with the Virtual Scribe and Ambient Speech Competitive Market Insights white paper.