Chore vs Core: Redefining Clinician Priorities for Enhanced Efficiency and Outcomes

Prioritizing Core Tasks Reduces Clinician Burnout and Improves the Patient Relationship
Should chores or core work take priority? The reality is that “chores” are still a priority, but they just don’t need to be a clinician’s priority. If it doesn’t have to be done by a clinician, it shouldn’t be. If it doesn’t have to be done in the exam room, it shouldn’t be. And if it doesn’t have to be done in a clinic, it shouldn’t be.
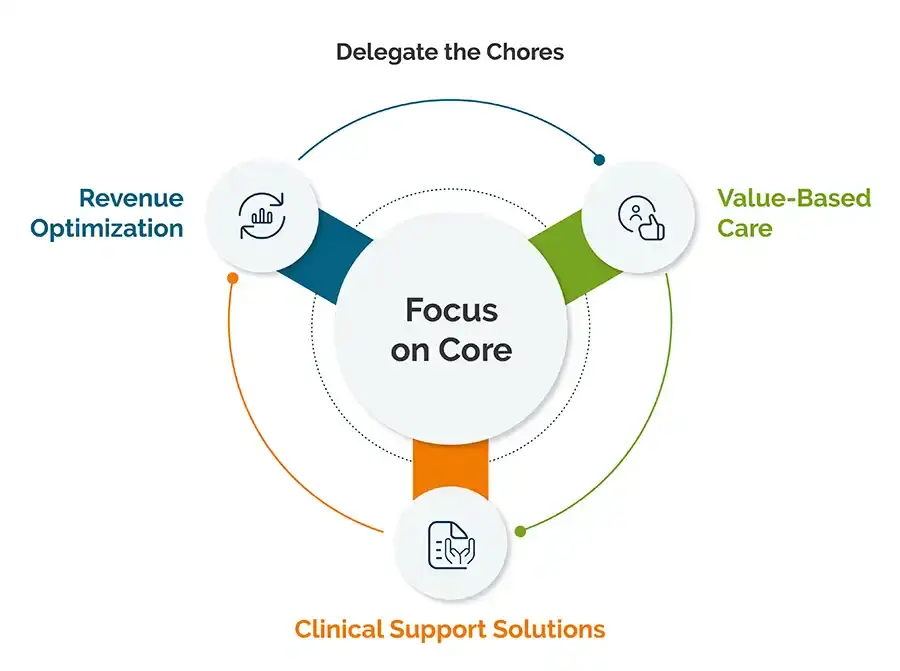
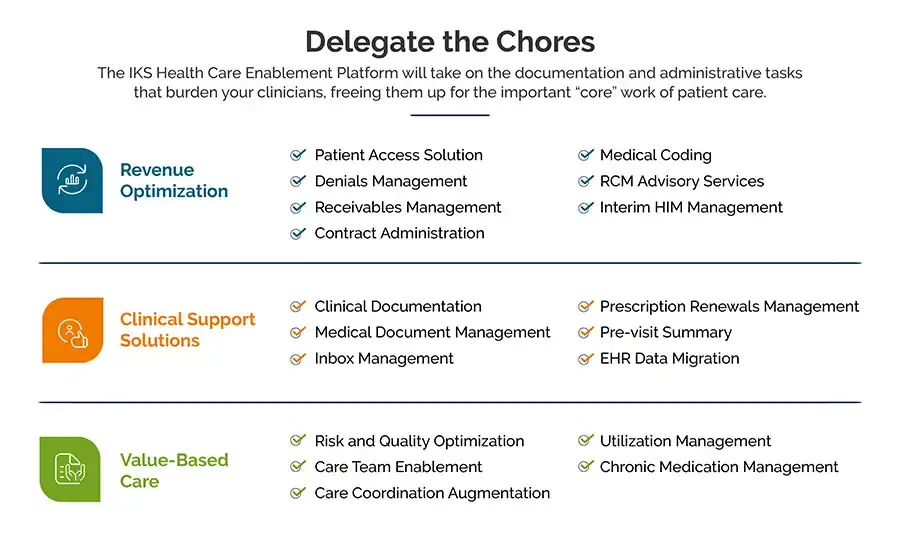
Let clinicians prioritize “core” tasks directly related to patient care and clinical outcomes, such as diagnosis, patient education, care coordination, and providing medical, surgical, and behavioral therapies. The chores, such as documentation, billing, administrative tasks, and other nonessential activities can be handled by someone else. Partnering with a company that specializes in these types of tasks means they often get completed faster and more accurately while allowing clinicians to provide better, safer, and more efficient patient care.
To achieve this, a redesign of the care delivery model that balances competing priorities effectively is needed. This involves rethinking workflows, leveraging technology, and employing a new approach to healthcare. The model of core vs chore outlines items that could be delegated outside of your clinical team in order to amplify patient care and bring joy back to the practice of medicine.
Identifying Chores: The Tasks That Burden Your Clinicians
Getting Priorities Straight Improves Clinician Wellbeing and Patient Care
Clinical documentation, managing the EHR inbox, coding and billing, prior authorizations, and other administrative tasks take time. All those minutes spent every day behind a computer screen instead of in front of a patient add up. According to Medscape’s “Physician Compensation Report” for 2023, physicians are spending 15.5 hours per week on paperwork and administration. Imagine what they could do with even a portion of that time back.
It’s been well documented that administrative burdens are causing burnout. The AMA reports studies showing the rise in burnout levels among U.S. physicians increasing from 38.2% in 2020 up to 62.8% in 2021. In addition to turnover, an article in the American Journal of Medicine lists other correlations from burnout, including:
- Decreased productivity
- Increased risk of major medical errors
- Poorer overall quality of care
- Decreased patient satisfaction and outcomes
- Suicidal thoughts
Shifting to Core Work Benefits Clinicians, Organizations, and Patients
It can sound too good to be true: Clinicians should focus on core activities. We have placed so many burdens on the shoulders of physicians that we’ve taken the joy out of practicing medicine. We need to put the doctor-patient relationship first, which means identifying and prioritizing core patient care responsibilities.
When it comes to reevaluating priorities, nothing is falling off the list – it’s simply moving from clinicians’ to-do lists onto someone else’s. A care enablement platform takes care of those chores for you. By using evolving AI technology with a human-in-the-loop approach, you can optimize your patient experience, practice operations, and revenue by preventing claim denials before they even happen.
This freeing up of time is instrumental in making an impact on their own health and enhancing patient care. Patients can feel heard and cared for again. Clinicians can have time to dive deeper into individualized care, treatment plans, and find their love for medicine again. Imagine what can happen when we enable our clinicians to focus on delivering great care instead of paperwork.
IKS Health is dedicated to helping you improve the experience of your patients, your clinicians, and your business. Discover what our Care Enablement Platform can do for your organization.